I recently published the above titled paper that highlights our results in treating lumbar herniated discs using regenerative medicine. This article was published in the current issue of The Journal of the American Osteopathic Association https://jaoa.org/article.aspx?articleid=2762063#.XlmK-1S638Y.email
To my knowledge, this is the first article that describes the use of an epidural used to address lumbar herniated discs. I cannot reproduce the paper for this purpose, but presented below is a more layman’s summary with two different case examples along with the references used for the publication.
The weight-bearing bones of the spine are separated by fluid-filled discs. If these discs bulge or herniate, there is a potential for pain as well as compression of the spinal. If nerve compression is severe, or prolonged, permanent nerve damage can ensue. There are several treatment options for herniated discs ranging from conservative (watchful waiting, Physical Therapy) to very invasive (surgery). If pain is a prominent symptom, we can try medications or epidural steroid injections to help reduce the inflammation contributing to pain and swelling. Sometimes, epidural steroid injections can reduce pain while the body tries to fix the lesion. It is well-established in the literature that the body can resorb, or “eat up”, these disc herniations, especially if they are large.
This resorption may take several months and the body may not resorb the herniation completely. During this process, it is important to monitor for unchanging or worsening symptoms. An objective measure we may employ during this time is using a nerve conduction test (EMG/NCS) to characterize the extent of nerve damage as well as the degree of recovery.
If pain, weakness, numbness/tingling or other neurologic symptoms are not improving, or are worsening, a more definitive intervention may be warranted. This may include surgery or a relatively safer procedure of injecting concentrated platelet growth factors (also known as platelet lysate) around the herniated disc. The two types of surgery include microdiscectomy (cutting away part of the disc) as well as spinal fusion (where the disc is removed entirely and hardware is placed to prevent movement at that segment). The drawback of a microdiscectomy includes the creation of a fresh wound that makes the disc susceptible to reherniation. Spinal fusion is a more invasive surgical approach requires a long recovery period and increases mechanical stresses in the segments adjacent to the fusion.
Injections of platelet lysate (PL) is a cutting edge therapy that has been a focus at our clinic. We have seen remarkable results with this treatment and have been able to spare numerous patients from having to resort to surgical alternatives. Platelets are rich in hundreds of proteins and growth factors that help facilitate healing. Installation of concentrated growth factors around a herniated disc can hopefully initiate, or accelerate, the healing process the body is trying to accomplish (but is perhaps doing a suboptimal job). This healing cascade can manifest through a variety of mechanisms that are directed by the signaling proteins in the platelet lysate.
The table below illustrates some of the general mechanisms by which these proteins work in the body. Delivery of these essential growth factors may be limited, perhaps because of a suboptimal blood supply that would inherently impair the conduit of platelets to the region of the herniated disc. We have been able to increase the concentration of growth factors around herniated discs by injecting PL via epidural injection.
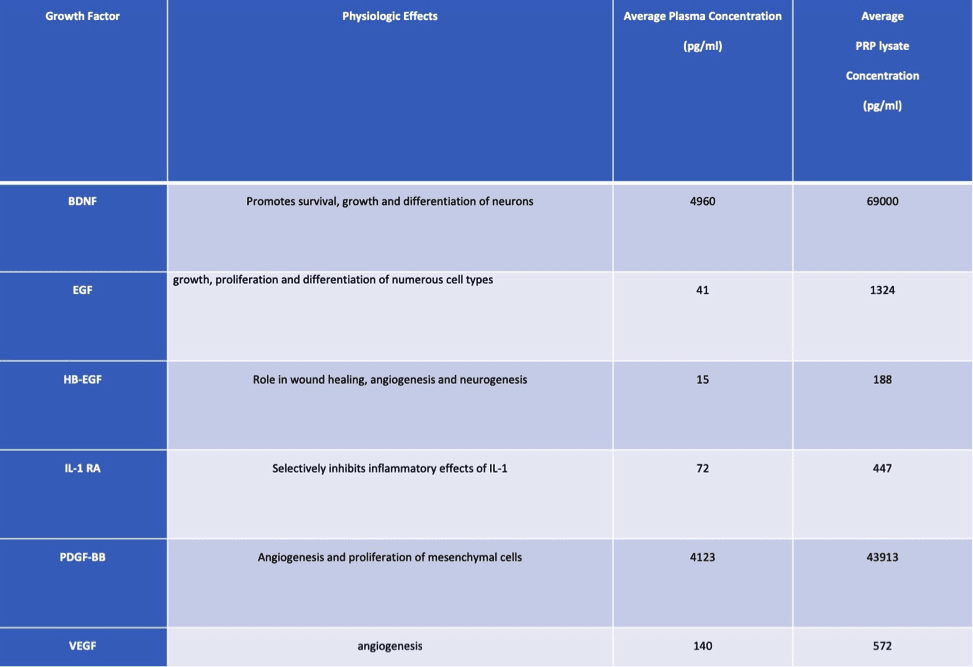
Figure 1:
Physiologic effects of selected growth factors found in plasma and PRP. Also shown is average growth factor concentrations produced by our laboratory compared to baseline levels. (pg/ml = picogram per milliliter, Bone-Derived Growth Factor (BDNF), Interleukin-1 Receptor Antagonist (IL-1 RA), Epidermal Growth Factor (EGF), Heparin-Binding EGF-like Growth Factor (HB-EGF), Platelet-Derived Growth Factor BB (PDGF-BB), and Vascular Endothelial Growth Factor (VEGF)).
Through independent research conducted through our clinic, and in collaboration from a university laboratory, we have discovered a proprietary technique of optimizing the concentration of growth factors that is significantly more robust compared to several widely established processing methods. The application of this research has shown in our clinical success stories. Below are a couple of case reports showing the power of this novel type of therapy.
CASE 1
The first case is of an 86-year-old gentleman who came to us with right leg pain numbness and weakness. We sent him for an MRI. The first two pictures show the large herniated disc that was compressing a nerve to his leg.

Image 1: Side view of the lumbar spine before treatment.
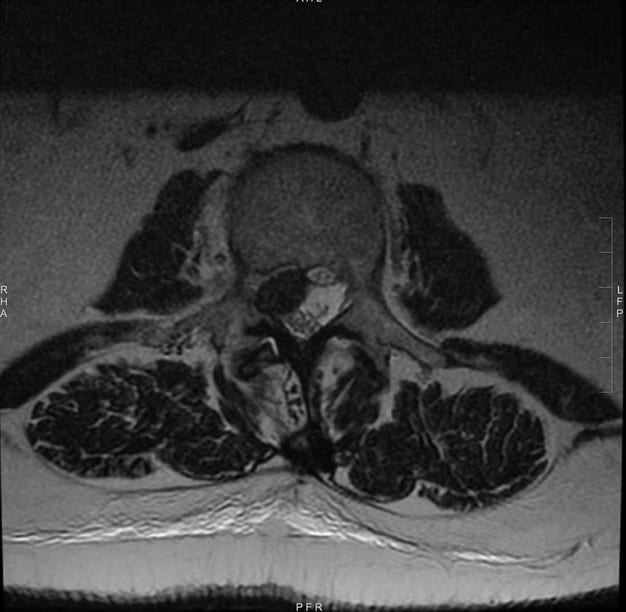
Image 2: Cross-section view of the lumbar spine before treatment.
His pain improved with an epidural steroid injection and he decided to pursue a conservative course of treatment with physical therapy for ongoing weakness and numbness. Despite three months of therapy, his weakness and numbness were worsening and his pain had returned. He was declining. We discussed surgery versus PRP to the lumbar spine with epidural growth factors (PRP/PL). He opted to pursue the PRP/PL injections. After two injections (about one month apart), he described improved function, decreased pain and improved strength. His numbness was improving, but still present. We repeated an MRI to monitor for progress and were happy to see the following results:

Image 3: Side view of the lumbar spine before treatment.
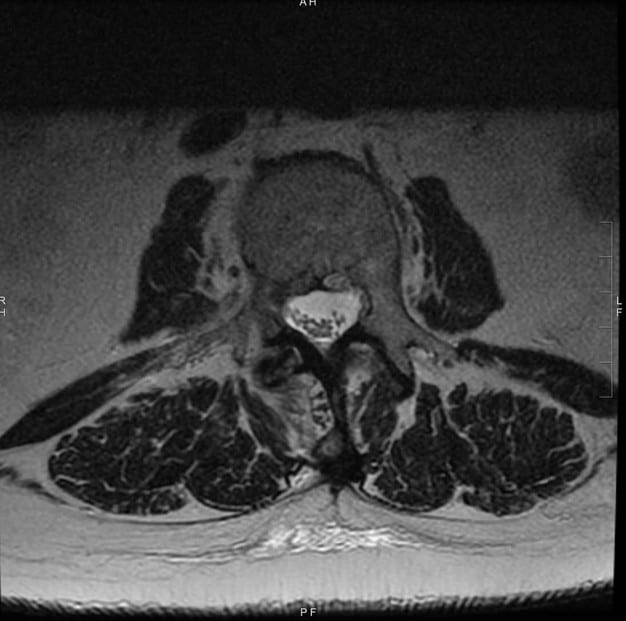
Image 4: Cross-section view of the lumbar spine after treatment.
It is obvious that there was a significant reduction in the size of the herniated disc. Ongoing care was left to an as-needed basis.
CASE 2
The next case involves a 48-year-old female who presented to me with severe neck and left arm pain along with profound weakness. We discussed surgery as an option, but she wanted to avoid this, so we proceeded with PRP to the cervical spine with epidural injection of platelet lysate.
After three total treatments, she had almost complete relief of pain and regained full strength. She was able to stop all pain medications and continues to be symptom-free years later. Below are comparison films from before and after treatments.

Image 5: Side view of the cervical spine before treatment. Note the impingement of the spinal cord.
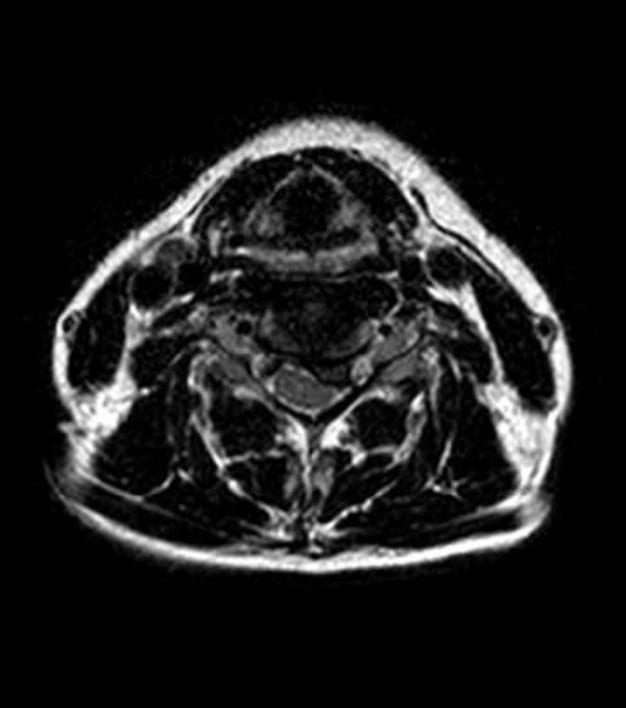
Image 6: Cross-section view of the cervical spine after treatment.

Image 7: Side view of the cervical spine after treatment.
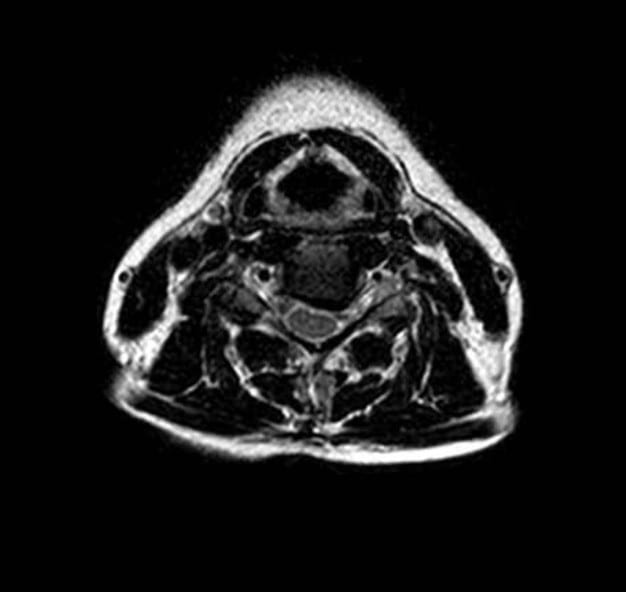
Image 8: Cross-section view of the cervical spine after treatment.
Through observation of clinical improvement and objective measures (including imaging), have found that epidural injection of concentrated platelet growth factors from platelet lysate has the potential to facilitate disc resorption. This, in turn, can help improve pain and function by decreasing the mechanical compression of the spinal nerves. While resolution of disc material can occur spontaneously, this process can take several months. Oftentimes, severe pain or neurologic compromise warrants a more aggressive approach to watchful waiting. Platelet lysate injections seem to be a safe alternative to opioids, s, and surgery. We have performed several hundreds of these procedures at CHARM. Many of the patients treated with this therapy report mild-to-moderate soreness at the PRP injection sites for generally less than 1 week after the procedure. In these situations a short course of oral pain medications is offered no other adverse events have been noted in any of the patients.
References
Rawson B. Platelet-Rich Plasma and Epidural Platelet Lysate: Novel Treatment for Lumbar Disk
Herniation. J Am Osteopath Assoc 2020;120(3):201–
207. doi: https://doi.org/10.7556/jaoa.2020.032.
Bicket MC, Chakravarthy K, Chang D, Cohen SP. Epidural steroid injections: an updated review
on recent trends in safety and complications. Pain Manag. 2015;5(2):129-146.
doi:10.2217/pmt.14.53
Kosztowski TA, Choi D, Fridley J, et al. Lumbar disc reherniation after transforaminal lumbar
endoscopic discectomy. Ann Transl Med. 2018;6(6):106. doi:10.21037/atm.2018.02.26
Wera GD, Dean CL, Ahn UM, et al. Reherniation and failure after lumbar discectomy: a
comparison of fragment excision alone versus subtotal discectomy. J Spinal Disord Tech.
2008;21(5):316-319. doi:10.1097/BSD.0b013e31813e0314
Parker SL, Mendenhall SK, Godil SS, et al. Incidence of low back pain after lumbar discectomy
for herniated disc and its effect on patient-reported outcomes. Clin Orthop Relat Res.
2015;473(6):1988-1999. doi:10.1007/s11999-015-4193-1
Lee JC, Choi SW. Adjacent segment pathology after lumbar spinal fusion. Asian Spine J.
2015;9(5):807-817. doi:10.4184/asj.2015.9.5.807
Benoist M. The natural history of lumbar disc herniation and radiculopathy. Joint Bone Spine.
2002;69(2):155-160.
Benson RT, Tavares SP, Robertson SC, Sharp R, Marshall RW. Conservatively treated massive
prolapsed discs: a 7-year follow-up. Ann R Coll Surg Engl. 2010;92(2):147-153.
doi:10.1308/003588410X12518836438840
Macki M, Hernandez-Hermann M, Bydon M, Gokaslan A, McGovern K, Bydon A. Spontaneous
regression of sequestrated lumbar disc herniations: literature review. Clin Neurol Neurosurg.
2014;120:136-141. doi:10.1016/j.clineuro.2014.02.013
Orief T, Orz Y, Attia W, Almusrea K. Spontaneous resorption of sequestrated intervertebral disc
herniation. World Neurosurg. 2012;77(1):146-152. doi:10.1016/j.wneu.2011.04.021