You have probably landed on this article because you are experiencing shoulder pain and looking for answers. You are not alone. Shoulder pain is thought to affect 30% of the world population and research shows that shoulder impingement syndrome accounts for up to 65% of all shoulder pain. In this article, we will examine the causes, symptoms, treatment options, and most importantly the prevention of shoulder impingement syndrome. If impingement is left untreated it can lead to more chronic tendon inflammation, injury, and progressive degenerative joint disease, but early intervention can significantly reduce this risk.
What Is Shoulder Impingement Syndrome?
The shoulder joint is the most freely moving in the entire human body, and as you can see in the anatomical image, there are tightly packed structures housed within this very mobile joint. Shoulder impingement occurs when the head of the humerus (upper arm bone) does not glide with proper mechanics within the glenohumeral (shoulder) joint when raising the arm, but instead bumps up into the acromion of the scapula (top of the shoulder blade) pinching the supraspinatus tendon of the rotator cuff, the subacromial bursa, or the biceps tendon.
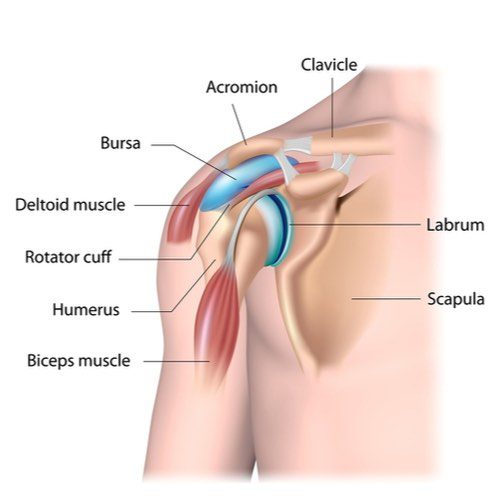
Primary impingement syndrome is defined when there is an anatomical abnormality of the acromion creating the lack of space for the humerus to glide within the glenoid fossa, but by far, the majority of shoulder impingement is secondary impingement syndrome. Secondary shoulder impingement syndrome is characterized by normal anatomy at rest with the onset of impingement and pain upon motion of the arm overhead, out to the side, or behind the back.
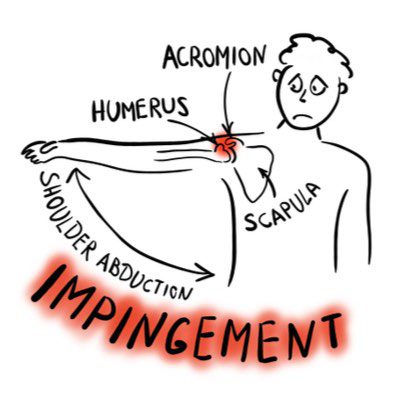
The causes of the common type of secondary shoulder impingement syndrome are often overuse, muscle weakness or imbalance, upper cross strain pattern postures or a combination of these factors.
Who Is At Risk For Shoulder Impingement Syndrome?
Anyone can be at risk for shoulder impingement syndrome, but it can frequently occur in overhead athletes or individuals who work repetitively with their arms up. Some examples of sports with a high prevalence of impingement are volleyball, baseball, softball, tennis players, and swimmers just to name a few. Shoulder impingement syndrome is so common in swimmers it will sometimes be referred to as “swimmer’s shoulder.”


Occupations at risk for secondary shoulder impingement syndrome are those who work with their arms up over their head or out to the side for extended periods of time like painters, construction workers, window washers, and hairdressers.
Causes Of Shoulder Impingment
So, let’s dive a bit deeper into the causes of shoulder impingement syndrome.
Overuse
Yes. Overuse is a common cause of impingement, but rarely is it overuse alone that creates a long-term problem. In addition to the sports, occupations, and recreational activities that create repetitive strain by using our arms above our heads, what else makes us susceptible to shoulder impingement?
Poor Posture
Why is posture so important to the health and function of our shoulders? I think a demonstration is the easiest way to answer this. Follow along and let’s explore.
- Sit or stand in a slumped over posture
- Maintain your rib cage and spine position
- Try to raise your arm up over your head
- How far did you get?
- Did you experience restricted motion in your shoulder?
- Feel tension, pinching, and/or discomfort?
Our shoulder girdle sits, virtually floats, in a sea of muscles atop our rib cage. For all the muscles to work effectively to meet the many demands we place on our shoulder joints; we must be working from a neutral rib cage and spine. Because many of the muscles that attach to the shoulder girdle and/or arm bone originate and are anchored to the rib cage and spine, the position or good posture is critical.
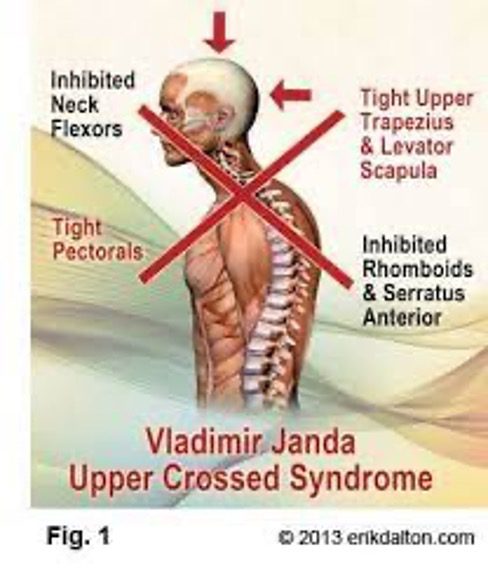
This common posture that is further exacerbated by hours of working slumped over a computer or cell phone is referred to as the upper cross strain pattern (UCSP). The UCSP brings with it a very predictable set of muscle imbalances that we will discuss further.
Muscle Tightness / Weakness / Imbalance:
The upper cross strain pattern is dominated by shortened and tight pectoralis muscles in the front of the chest, the SCM muscles in the front of the neck, and sub-occipital muscles at the base of the skull, as well as lengthened and tight upper trapezius and levator scapulae in the upper back and posterior neck. The other half of the cross-pattern is inhibition and weakness of the deep neck flexors and a number of muscles in the mid-back namely the serratus anterior, rhomboids, mid and lower trapezius.
A balance of the muscles that stabilize the scapula (shoulder blade) is vital to proper biomechanics at the glenohumeral joint and limits the risk of shoulder impingement, degenerative joint disease, and rotator cuff injury.
Core strength and neutral stabilization of the rib cage and spine are also critical. As we mentioned above, all the muscles that balance and stabilize the shoulder girdle are attached to the rib cage and spine and are therefore vital to proper mechanics during overhead activities and sports. In addition to affecting the mobility of the shoulder, insufficient core strength and stability will impair the transfer of forces through the body, across the shoulder girdle, and out the length of the arm. To avoid unnecessary strain and injury to the shoulder, elbow, wrist, and hand, focus on the core is essential.
Symptoms of Shoulder Impingment
Symptoms often come on gradually and are not readily attributed to one single event. Common signs and symptoms of shoulder impingement include:
- Pain when lifting, reaching or lowering your arm from an overhead position
- Pain in the front of your shoulder
- Shoulder or arm weakness/stiffness
- Decreased range of motion
- Pain lying on the affected side
- Pain that radiates from the shoulder down the side of your arm
- Aching pain at night affects your sleep
- Pain reaching behind your back
This list is self-explanatory and not exhaustive, but if you are experiencing symptoms lasting more than a couple of weeks or ones that seem to recur and linger, then it would be a good idea to get that shoulder checked out.
Testing For & Diagnosing Shoulder Impingement
A comprehensive history, physical exam, and functional movement assessment by a doctor or physical therapist who specializes in the shoulder will often give you all the answers you need. Common areas of tenderness and frequently painful motions discussed above can be accompanied by specific tests for diagnosing shoulder impingement syndrome including:
- Hawkins Test
- Neer Sign
- Jobe test
- Painful Arc of Motion
Hawkins Kennedy Test
- Position into 90 degrees forward flexion and 90 degrees elbow flexion
- Support the patient’s arm with a hand on the opposite shoulder
- Passive internal glenohumeral rotation
- The test result is positive if you experience any pain or apprehension
Neer Sign Test
- Stabilize at acromion (top of shoulder)
- Internal rotation at the glenohumeral joint
- Passively move the arm into flexion overhead
- The test result is positive if you experience pain
Jobe’s Test “Empty Can Test”
- Passive Abduction to 90 degrees.
- Bring into scapular plane of flexion.
- Internal glenohumeral rotation.
- Ask the patient to actively hold the position.
- Resist position asking the patient to hold against this resistance.
- The result of the test is positive if the patient is unable to hold the arm against the resistance or pain is provoked
Painful Arc of Motion Test
- The patient is instructed to actively elevate their arm into overhead abduction.
- Then slowly reverse the motion
- The result of the test is considered positive if the patient experiences pain between 60-120 degrees of elevation.
Instability of the shoulder joint itself should also be assessed especially if there has been any specific trauma, sports or overuse history, or long-standing pain. Since the shoulder is such a mobile joint with high degrees of freedom, treating both the underlying structural instability and functional neuromuscular control deficits should be addressed. More on that when we get to treatment options.
Determining the severity of the injury is important in diagnosis and treatment. Neer classified three categories or stages according to the severity of impingement syndrome. Stage I impingement primarily results from irritation and inflammation and is classically seen with overuse-type mechanisms resulting in tendonitis or bursitis. Stage II is characterized by greater degenerative changes resulting in tendinopathy or tendinosis. A rupture or tear of the tendon may result from chronic, longstanding injury to the tissue and is seen in Stage III shoulder impingement syndrome.
If the severity of shoulder impingement syndrome is at Stage II or III the use of Diagnostic Ultrasound or Magnetic Resonance Imaging (MRI) can greatly assist in determining how much tissue damage has been done and will help steer the best combination of treatment options.
You can find more information about tests and shoulder impingement classifications at the National Library of Medicine.
Conservative Treatment Options For Shoulder Impingement
Conservative treatment is not only appropriate with a Stage I shoulder impingement but critical during all stages to complement other treatments for full recovery of function and to decrease the risk of re-injury. It is helpful to take a release, balance, build approach to shoulder impingement syndrome.
Release
The first thing we need to do is to stop irritating the tissue. As discussed earlier, the shoulder is a highly mobile and closely packed structure. Releasing tight and over-active muscles especially through the pectoralis, latissimus, and long head of the triceps can all be very helpful. Some common techniques include manual therapy, direct pressure release techniques, dry needling, microcurrent point stimulation, and use of percussion devices.
My personal favorite is the HyperVolt!
Inflammation causes additional compression and worsens the impingement of sensitive tissues. Reducing the inflammation can rapidly decrease pain and further irritation with some common strategies being ice, over-the-counter anti-inflammatory medication like ibuprofen, Class IV Laser Therapy, prescription medication, and steroid injections which will be detailed a bit later.
If repetitive overuse is the primary cause of the impingement, then some rest or time off from that sport/activity may be necessary.
Balance
A physical therapist experienced in the shoulder can assist you in functional treatment options that focus on improving the muscle balance and strength through the posterior shoulder girdle, scapula, and glenohumeral joint to decrease impingement and pain. There are many approaches, but it all boils down to improving joint position, biomechanics during motion, strength (especially the serratus anterior, rotator cuff, mid and lower trapezius), endurance, and stability during activities. Treatment strategies may be similar in the release, balance, and build components, but the actual program will depend on the loads and demands individuals place on their shoulders.
A revolutionary way to identify what muscles are either being blocked from working (inhibited) or being abnormally called into tension (over-facilitated) due to protective responses mediated by the brain, is the use of Neubie (Neuro – Bio – Electric – Stimulation). Through a Neubie scan followed by guided functional exercise while under the application of high-frequency direct current, we can provide enormous input to the nervous system. The goal is to change how the brain responds to load so activation of muscles and proper motor patterns are no longer seen as threatening. This therapy combined with selective exercise or sports-specific drills can quickly and dramatically improve neuromuscular control across the shoulder girdle.

As we discussed earlier, neutral posture and the optimal shoulder joint position that follows is critical for successful shoulder rehabilitation, reducing the risk of re-injury, and a positive long-term functional outcome.
Build
Just to re-emphasize, the shoulder is a highly mobile joint that manifests much of its functional strength, power, and performance during pushing, pulling, swinging and throwing through the summation of forces from the ground through the entire kinetic chain, and the inherent structural and neuromuscular stability across the shoulder girdle and glenohumeral joint. You can appreciate the transfer of forces from the ground through the legs, pelvis, core, shoulder girdle and arm in the photo below of the javelin throw.
We can address strengthening through resistance training in an open kinetic chain with bands, dumbbells, and machines, as well as the use of body weight-bearing exercises in closed kinetic chain exercise with push-ups, pull-ups, and suspension training using tools such as the TRX or Redcord. The suspension provides high proprioceptive input and challenges individual joint, girdle, and multi-segmental core stabilization in a different way than exercise on stable surfaces. Full kinetic chain integration for joint protection, optimal shoulder function, stability, and performance is critical in building the strength and power needed to meet imposed demands from basic activities of daily living to high-level sports performance.

We have covered some of the therapeutic basics of conservative intervention for shoulder impingement which will be shared in videos at the end of this article. These same approaches can be used in conjunction with medication management, injection strategies, and rehabilitation following a surgical procedure. Let’s dive into those treatment strategies next.
NSAIDs and Steroids
Your physician may suggest prescription medications to treat shoulder impingement again with the goal of reducing inflammation and pain. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) are commonly prescribed or used as over-the-counter options. These include ibuprofen (Advil), Naprosyn (Aleve), and several prescription medications, such as Meloxicam, Celebrex, and others. Although initially helpful for acute pain and swelling, there are significant side effects including stomach irritation and ulceration, kidney injury, increased risk of heart damage, and excessive bleeding. These risks increase when these medications are used chronically. These medications are indicated for short-term use, but many patients assume that they are safe to take chronically because they can be purchased over the counter. Unfortunately, many hospitalizations and deaths occur every year due to chronic overuse of NSAID medications.
For more info on NSAID complications view the safety announcement from the FDA.
Corticosteroid medications such as Prednisone may also be taken orally or by injection but also have limitations and side effects. These have significant risks including immune system inhibition, stomach irritation and ulceration, mood effects including depression and anxiety, and weakening of the connective tissues when overused, even at times leading to tendon rupture and worsening of partial tendon and ligament tears. Corticosteroid injections have been proven to damage cartilage cells in joints. Repeated injections of steroids into joints will likely produce more harmful than beneficial effects. Steroid injections also have a significant risk of infection because they reduce the immune system response in the tissues that they are injected into. Injections that are too concentrated or too superficial may also damage the skin and fat tissues, sometimes leaving pitted areas in the skin and bleaching the color of the skin, especially in darker-skinned patients. With all the risks noted, it is important for the patient and the physician to be mindful of the side effects of steroid injections and use them sparingly, if at all.
For more information on the dangers and potential complications of corticosteroid injections visit the link from WebMD here.
Regenerative Medecine
Stem Cells & Platelet-Rich Plasma Therapy
A Non-surgical Regenerative Medicine to Treat Shoulder Impingement Syndrome
Regenerative medicine focuses on improving the structural stability of the ligaments and the shoulder joint capsule, while also strengthening the tendons and myofascial attachments. Injections of growth factors into the damaged tissues, using Platelet Rich Plasma (PRP) and Stem Cells from Bone Marrow Aspirate Concentration (BMAC), have been shown to regenerate and repair the degenerative and torn connective tissues. The growth factors from Platelets and Stem Cells improve local blood flow to bring in more nutrients, and they communicate with other neighboring cells including fibroblasts, macrophages, local stem cells, and other cells to coordinate the repair process. As these tissues become healthier, the instability, limited range of motion, and muscle inhibition that is commonly seen in shoulder impingement syndrome is reduced or eliminated, and shoulder function is more likely to optimally respond to the physical therapy interventions we discussed earlier.
This is how it’s done. Platelets and Stem Cells are removed from the patient on the day of the treatment using minimally invasive techniques and are then precisely re-implanted at the sites of degeneration and injury using X-Ray fluoroscopy and ultrasound guidance to stimulate healing of the weakened tissue. The entire process occurs over about 2 hours in an outpatient clinic, and patients can return home and continue their normal activities when the procedure is completed. Regenerative medicine procedures are well-tolerated and normal activity is encouraged. Pain, soreness and swelling after regenerative medicine is expected for about 2-4 days, or at times, up to about a week. Usually, the procedure will need to be repeated about every 1-2 months for a total of 2-4 treatments.
Surgical Intervention
The surgical approach for shoulder impingement is based on the idea that increasing the limited space for the rotator cuff tendons seen on X-Ray and MRI Scans will be beneficial. Unfortunately, the limited space observed on MRI and X-Rays is often deceptive. These studies are static and often do not reflect how the structures actually move when activated. When there is shoulder capsule ligamentous weakness, the shoulder will often “ride high” in the subacromial space. When the rotator cuff tendons are injured, the rotator cuff muscles are inhibited, which then allows the glenoid to rise within the space when the arm is elevated, and “crimp” the tendons, causing further tendon constriction and degeneration. Weak and degenerative ligament and tendon structures are usually the core cause of shoulder pain.
Shoulder decompression surgery involves the removal of bone from the acromioclavicular joint, the acromion, and the clavicle (collarbone), and may be recommended in severe cases of bony impingement causing compression and severe tearing of the tendons within the subacromial space. This can be successful in severe cases of impingement with associated complete tendon tears, but it is often recommended in less severe cases in which the compression is dynamic and would otherwise respond to physical therapy and regenerative injections. Sometimes shoulder joint replacement might be needed if there is severe arthritic joint cartilage degeneration.
There are significant risks of shoulder surgery, including infection, re-rupture of repaired tendons and of the glenoid labrum, worsened instability of the shoulder capsule, worsened arthritis and cartilage injury, prolonged pain for 3-6 months or longer, and prolonged recovery, which often consumes 6-12 months of intensive rehabilitation after surgery. Surgery should be considered only as a later option after non-surgical approaches (Advanced Physical Therapy, Regenerative Medicine Injections) have been unsuccessful at improving the integrity and function of the shoulder.
An Ounce of Prevention
In this article, we discussed how shoulder impingement syndrome is best treated with a combination approach including neuromuscular-based exercise to address functional biomechanics and many times regenerative medicine to address structural joint integrity. Many commonly used interventions can reduce pain but do not address the root cause of the impingement and can be detrimental to local tissue and systemic health over time.
As with most aspects of healthcare, an ounce of prevention is worth a pound of cure and taking care of our shoulders is no exception. We live in a world that no longer demands the same daily range of motion, strength, or weight-bearing stability of our upper body as it once did. These “conveniences” have created strain and weakness/inhibition patterns that require just a few minutes a day to combat. Below are three videos that outline just a few of many foundational exercises that address rotator cuff strengthening, serratus anterior stabilization in pushing, and mid/lower trap and rhomboid stabilization when pulling. Remember to release, balance, and build your way to happy and healthy shoulders for a lifetime.
Rotator Cuff
Serratus Anterior
Middle & Lower Trapezius

Michele Zink Harris
PT, CNP, RASDepartment of Physical Therapy
Center For Healing & Regenerative Medicine