The anterior cruciate ligament (ACL) is a major stabilizing ligament in the knee. Rupture of the ACL can lead to significant pain, functional deficits and accelerated joint degeneration due to knee instability. Tissues such as cartilage, tendons and ligaments have inherent limitations in healing and regeneration. This is, in part, due to the avascular nature of these tissues. So, spontaneous tissue repair is akin to growing crops in a dessert. Subsequently, ACL tears and ruptures are not thought to heal spontaneously. Because of this, even small tears can lead to a chronically deficient structure with the potential for increased tissue damage. Surgical reconstruction is the current standard of care ruptured ACLs. This is a valuable technique where a surgically implanted graft generally provides improved stability and joint protection, but it is not without potential sequelae. This surgery often leads to impaired proprioception (how we sense where a body is in space), along with altered mechanics. These changes can lead to early, and accelerated, degenerative changes in the knee joint.
This creates a treatment gap between non-treatment that leads to chronic instability and surgical repair that precipitates biomechanical dysfunctions. More recently, use of therapies have been proposed to help fill this treatment gap. With this strategy, injections of biologic agents, such as autologous platelet rich plasma (PRP) and/or bone marrow aspirate concentrate (BMAC), have been used to promote tissue repair in tissues that otherwise show limited ability to heal on their own. Centeno, et al showed good evidence for repair of ACL tears where the ruptured tissue ends have close approximation to each other. They describe criteria of less than 1cm of retraction space between the ends of the ruptured ACL segments. Described below is a case of ACL repair using bone marrow aspirate concentrate and platelet-rich plasma in a situation where the ACL fibers showed significant separation.
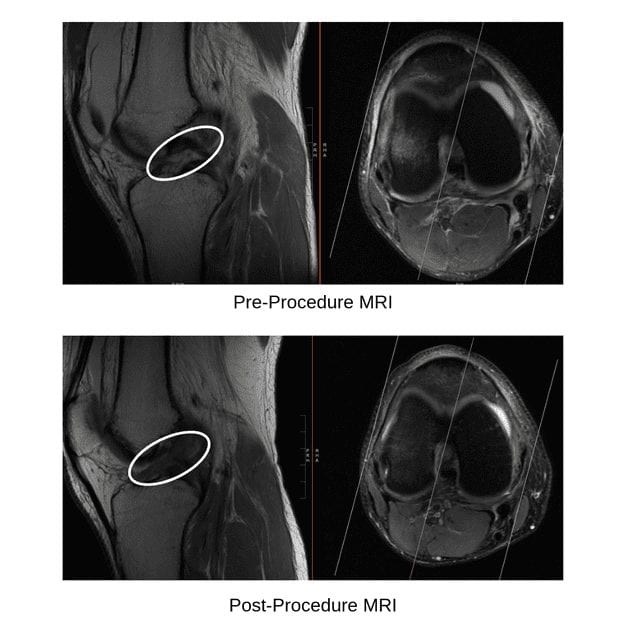
The patient is a 29-year-old male presented to our clinic with right knee pain and swelling that began after a fall while wakeboarding. MRI revealed a complete rupture of the ACL with > 20mm separation of the free fragments (figures 1, 2). He had a previous left ACL repair with a prolonged recovery and a suboptimal clinical outcome due to ongoing pain and instability. Because of this, he wanted to explore non-surgical options for his right knee injury. He opted to pursue autologous BMAC/PRP treatments.

We performed two BMAC/PRP treatments using fluoroscopic (X-ray) guidance to ensure proper placement. The treatments were 3 weeks apart. A repeat MRI was performed 4 weeks after the second treatment. The repeat MRI showed interval healing of the anterior cruciate ligament with continuous fibers seen throughout its course (figure 3). Examination showed good ligamentous stability and very little pain. He had returned to most functional activities without limitations.
This case demonstrates excellent structural improvements with injection of autologous BMAC/PRP to the ruptured ACL.
Treatment with autologous BMAC and PRP is a same day procedure intended to accentuate, or initiate, the body’s natural healing processes. Although there is expected post-procedure soreness, this treatment is considered very safe and generally does not exclude other treatment options if failure. Surgical reconstruction remains the gold standard for ACL ruptures, however this is not without potential drawbacks. This case illustrates the need for further research evaluating the use of biologic treatments for orthopedic injuries such as ACL repair.
Regenerative medicine treatment of ACL ruptures may help fill the treatment gap between non-treatment, or bracing alone, and surgical reconstruction.
Ben Rawson, D.O.